

To operate a centre of excellence which improves access to quality, evidence-based palliative care for patients and families in need through delivering an integrated clinical service, carrying out research, advocacy, training and capacity building, in collaboration with partners.


Each of GlobalGiving’s nonprofit partners is required to send quarterly donor reports detailing the impact of their work. Here are some of their recent updates:
By Grace Kivumbi | Project manager
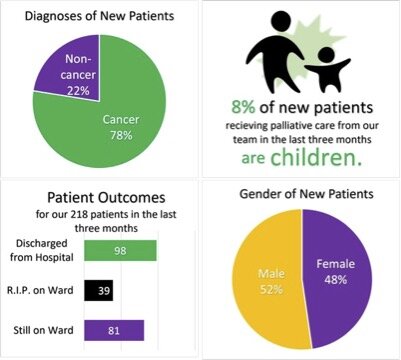
In the three months of October, November, and December 2023, our clinical team, including social worker volunteers have continued to provide care to our patients in both the Mulago National Referral... Read the full report ›By Grace Kivumbi | Project Manager
Clinical care and relationships In the three months of July, August, and September our clinical team, including social worker volunteers, visited our patients 1,024 times. We also contacted them by... Read the full report ›By Grace Kivumbi | Project Administer
We are delighted to share with you our second report this year, we thank all our supporters from Uganda and around the globe. The year is progressing well with our services including patient care for... Read the full report ›